- Protruding Foreign Body Toolkit
There may be nothing more disconcerting than being confronted with a patient with a penetrating foreign body protruding from the head. Careful planning and understanding of the altered anatomy associated with this injury is critical. It is also worth reminding that first principles associated with Advanced Trauma Life Support must be prioritized appropriately. "Gory" injuries can distract physicians and cause deviations from the ABCs and standard ATLS procedures and processes. This must be avoided.
The proposed algorithm starts with general management principles. Many protruding foreign bodies require stabilization to ensure that they do not move within the skull causing further injury to the brain. In general, all protruding penetrating foreign bodies will require removal, and intervention should proceed as soon as safe and feasible. It is specifically recommended that the foreign body be removed in an operating room or similar controlled environment by a neurosurgeon or their designee. This is predominantly so that resources are available to address hemorrhage from a recognized or unrecognized vascular injury. There is a strong association between protruding foreign bodies and possible vascular injury
12,19,20,58 . Obtaining appropriate vascular imaging is critical to avoid potential catastrophic blood loss, and the Penetrating Vascular Injury algorithm should be consulted. A proximal injury to a large artery at the skull base may require endovascular intervention prior to FB removal.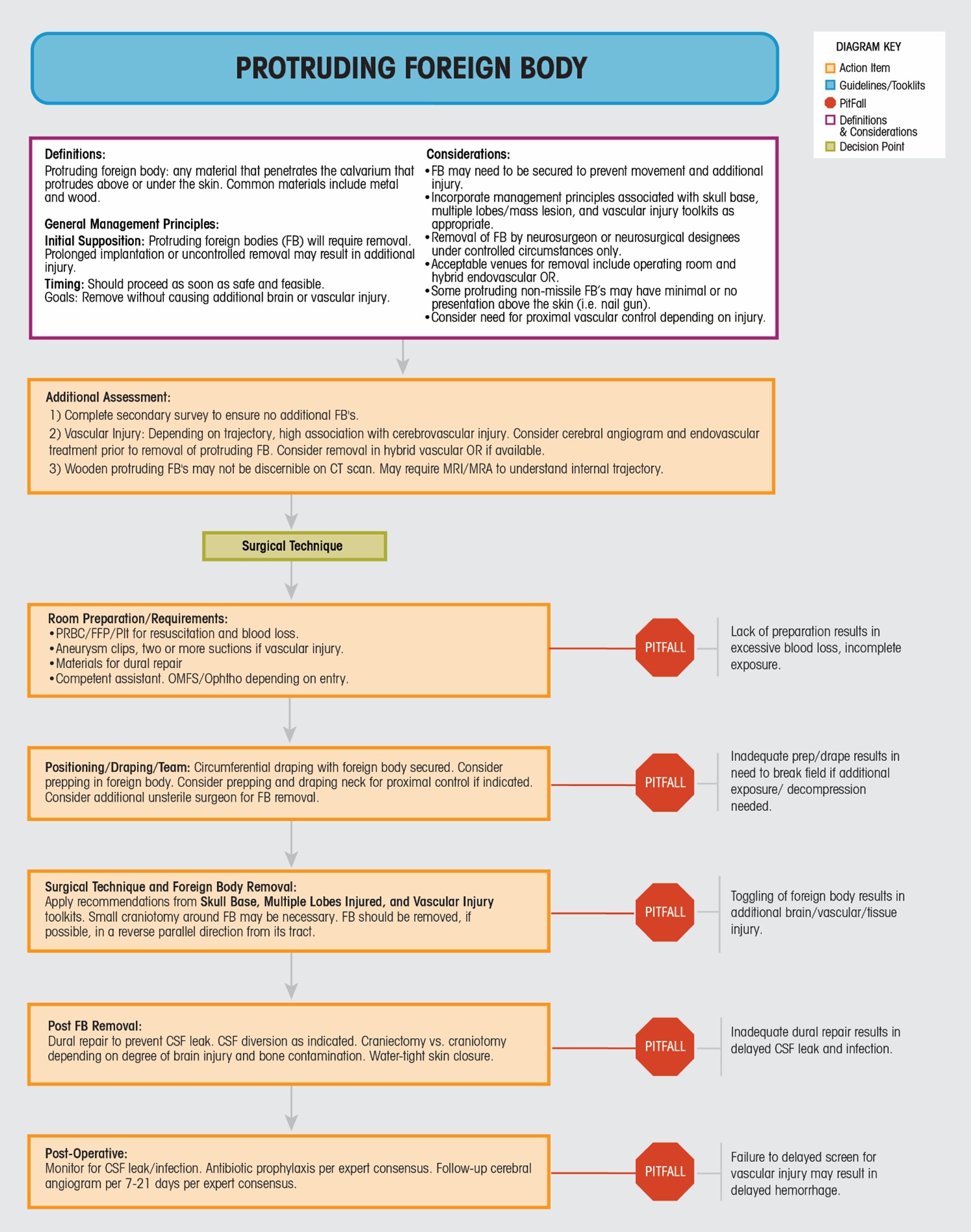
We favor removal of a penetrating foreign body after open or endovascular surgery has achieved access to proximal vessels which made bleed profusely following removal of the foreign object. We are aware of a described practice whereby such foreign bodies are removed in a controlled environment without such proximal control established. In such a paradigm CT and angiographic imaging is obtained immediately after object removal and surgical or endovascular management are emergently performed if needed. Our group has a preference to only remove such foreign bodies in conjunction with open or endovascular surgeries but in the absence of strong evidence informing the approach, the comfort, wisdom and experience of the treating team should play a key role in determining specifically how a foreign body is removed.
Concerning operative interventions, specific requirements should be dictated by the location of penetration. For example, a penetrating orbital injury may be associated with skull base disruption. A multi-disciplinary team including ophthalmology or oro-maxillo-facial surgery may be necessary to safely address removal and repair. Aneurysm clips with thought concerning proximal control is also recommended.
Positioning and draping should take into account the protruding FB and plans for removal as well as surgical approaches that may be needed to achieve proximal vascular control. For instance the neck may have to be prepped and draped. A craniotomy may be necessary, and the extent of this opening should take into account the possibility of craniectomy if significant associated brain injury and swelling is encountered. Once operative control of the FB and possible vascular injury has been established, the FB should be removed in the opposite and parallel direction of insertion with minimal toggling to avoid additional injury. A non-sterile individual can remove the object or in some instances the protruding object can be covered with a sterile material to facilitate removal by the sterile operating team. Some objects embedded in bone can require great force to remove and sometimes drilling away this bone. Following removal, and as applicable, standard dural and possibly skull base repair (see Skull Base Injury Toolkit) should proceed with every effort made to reduce the likelihood of cerebrospinal fluid leak. This may include placement of an external ventricular drain.
Post-operatively, it Is important to monitor for CSF leak and rectify if this occurs. CSF leak in this setting generally occurs with inadequate dural repair or increased intracranial pressure, and is associated with the development of delayed infection (Section VII-4, Prevention and Management of Cerebrospinal Fluid Leaks, Level II)
53,59-72 . Antibiotic prophylaxis should proceed in a manner recommended by Expert Consensus (VIII-4 Antibiotic prophylaxis)58,73 recognizing that these wounds are inherently contaminated. A follow up cerebral angiogram is generally necessary to exclude the delayed development of traumatic pseudoaneurysms, and is especially important if arterial injury is encountered or if the trajectory of the FB traversed an arterial territory, and should occur sometime during the 7-21-day period following repair (VI-7 Neurovascular Imaging; VII-7 Endovascular Management of Traumatic Aneurysms). - Protruding Foreign Body Toolkit
There may be nothing more disconcerting than being confronted with a patient with a penetrating foreign body protruding from the head. Careful planning and understanding of the altered anatomy associated with this injury is critical. It is also worth reminding that first principles associated with Advanced Trauma Life Support must be prioritized appropriately. "Gory" injuries can distract physicians and cause deviations from the ABCs and standard ATLS procedures and processes. This must be avoided.
The proposed algorithm starts with general management principles. Many protruding foreign bodies require stabilization to ensure that they do not move within the skull causing further injury to the brain. In general, all protruding penetrating foreign bodies will require removal, and intervention should proceed as soon as safe and feasible. It is specifically recommended that the foreign body be removed in an operating room or similar controlled environment by a neurosurgeon or their designee. This is predominantly so that resources are available to address hemorrhage from a recognized or unrecognized vascular injury. There is a strong association between protruding foreign bodies and possible vascular injury
12,19,20,58 . Obtaining appropriate vascular imaging is critical to avoid potential catastrophic blood loss, and the Penetrating Vascular Injury algorithm should be consulted. A proximal injury to a large artery at the skull base may require endovascular intervention prior to FB removal.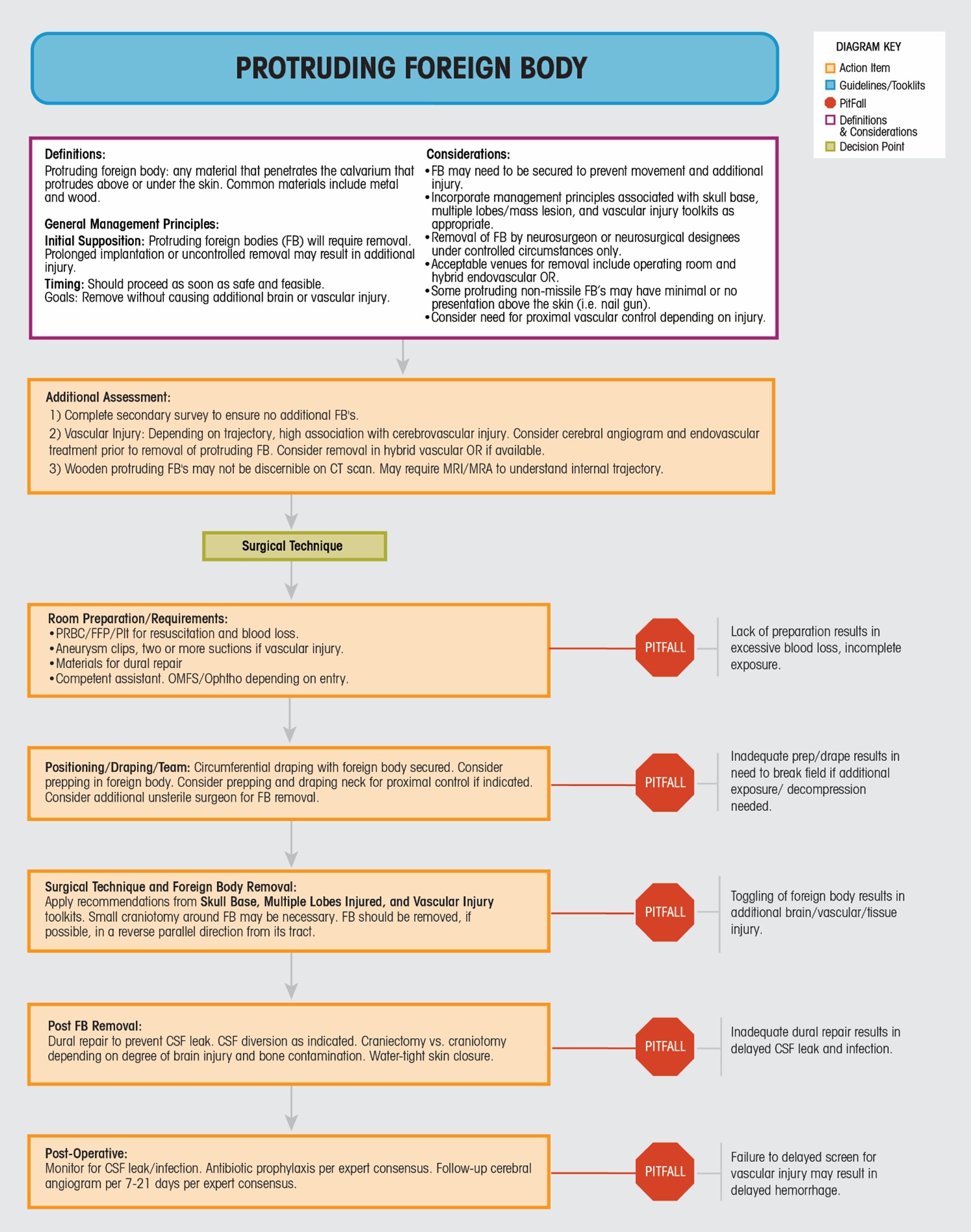
We favor removal of a penetrating foreign body after open or endovascular surgery has achieved access to proximal vessels which made bleed profusely following removal of the foreign object. We are aware of a described practice whereby such foreign bodies are removed in a controlled environment without such proximal control established. In such a paradigm CT and angiographic imaging is obtained immediately after object removal and surgical or endovascular management are emergently performed if needed. Our group has a preference to only remove such foreign bodies in conjunction with open or endovascular surgeries but in the absence of strong evidence informing the approach, the comfort, wisdom and experience of the treating team should play a key role in determining specifically how a foreign body is removed.
Concerning operative interventions, specific requirements should be dictated by the location of penetration. For example, a penetrating orbital injury may be associated with skull base disruption. A multi-disciplinary team including ophthalmology or oro-maxillo-facial surgery may be necessary to safely address removal and repair. Aneurysm clips with thought concerning proximal control is also recommended.
Positioning and draping should take into account the protruding FB and plans for removal as well as surgical approaches that may be needed to achieve proximal vascular control. For instance the neck may have to be prepped and draped. A craniotomy may be necessary, and the extent of this opening should take into account the possibility of craniectomy if significant associated brain injury and swelling is encountered. Once operative control of the FB and possible vascular injury has been established, the FB should be removed in the opposite and parallel direction of insertion with minimal toggling to avoid additional injury. A non-sterile individual can remove the object or in some instances the protruding object can be covered with a sterile material to facilitate removal by the sterile operating team. Some objects embedded in bone can require great force to remove and sometimes drilling away this bone. Following removal, and as applicable, standard dural and possibly skull base repair (see Skull Base Injury Toolkit) should proceed with every effort made to reduce the likelihood of cerebrospinal fluid leak. This may include placement of an external ventricular drain.
Post-operatively, it Is important to monitor for CSF leak and rectify if this occurs. CSF leak in this setting generally occurs with inadequate dural repair or increased intracranial pressure, and is associated with the development of delayed infection (Section VII-4, Prevention and Management of Cerebrospinal Fluid Leaks, Level II)
53,59-72 . Antibiotic prophylaxis should proceed in a manner recommended by Expert Consensus (VIII-4 Antibiotic prophylaxis)58,73 recognizing that these wounds are inherently contaminated. A follow up cerebral angiogram is generally necessary to exclude the delayed development of traumatic pseudoaneurysms, and is especially important if arterial injury is encountered or if the trajectory of the FB traversed an arterial territory, and should occur sometime during the 7-21-day period following repair (VI-7 Neurovascular Imaging; VII-7 Endovascular Management of Traumatic Aneurysms).
